A multi-part series on challenges and solutions to better medication adherence
As former Surgeon General Regina M. Benjamin, MD, MBA, has said, we can’t begin to address prevention — the foundation of the health of each patient and the nation as a whole — if patients don’t understand what we’re trying to explain to them. So improving the nation’s health literacy is critical to creating a system of care based on wellness and prevention that delivers the kind of clinical, financial and satisfaction outcomes we all want.
An adequate level of health literacy is just plain essential to medication adherence. Especially as most people age, there are typically more and more conditions faced by patients, and more new and/or established brand and generic drug names and potential side effects to fully comprehend. Even the basic terms that can impact a patient’s life — insulin, Type 2 diabetes vs. Type 1, hypertension, and more-complex ones such as phenylketonuria or pneumoconiosis — take time, patience and expert assistance for most patients to fully comprehend.
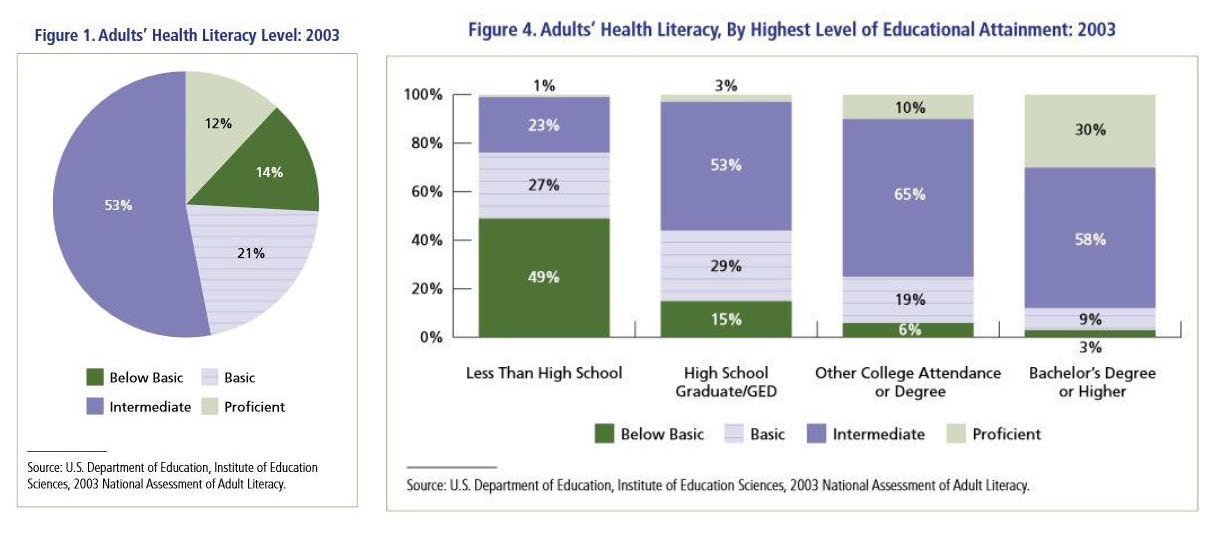
Only 12% of adult patients ‘get you’…meaning 88% do not
Unfortunately, the statistics for U.S. health literacy are sobering. Only 12% of U.S. adults have proficient health literacy, according to the NAAL study published by HHS’ Office of Disease Prevention and Health Promotion. More than a third of adults were in the basic (47 million) and below-basic (30 million) categories for health literacy. Over half of adults had intermediate health literacy skills at best. According to the Centers for Disease Control and Prevention (CDC), some lack of health literacy affects 9 out of 10 adults who struggle to understand complex or unfamiliar health information.
So here’s the bottom line: As clinicians, what we say doesn’t matter unless our patients are able to understand the information we give them well enough to use it to make good healthcare decisions. Otherwise, we didn’t reach them, and that’s the same as if we didn’t consult with them or treat them at all.
One of the six ‘buckets’ that affect nonadherence
In our consults, RxLive’s clinical pharmacists see this wide disparity of knowledge and comprehension every day. Thus, by combing our own deep knowledge and experience with a thorough review of peer-reviewed literature, our team has included it in what we call six major “buckets” of the causes of medication nonadherence that we work to uncover and address. These are covered in a multi-part series of blogs including this one:
- Understanding and knowledge (health literacy)
- Side effects
- Cost
- Skills
- Social and behavioral factors (both external and internal)
- Access to care and burden of the regimen
Using the RxLive technology platform, whenever a pharmacist identifies a potential medication-adherence problem, they can click that reason in the drop-down to receive a suggestion about addressing that adherence issue. This adds to their own extensive knowledge as they address medication-adherence issues with each patient.
The impact of health illiteracy
The Institute of Medicine (IoM) describes health literacy as the ability of an individual to make appropriate health decisions according to the extent of their capacity to obtain, communicate, understand and use health information. Health literacy requires an assortment of skills — reading, listening, communication, comprehension, analytical and numeracy — to execute a medication regimen.
Inadequate health literacy skills impede patients’ ability to build knowledge about their illness and therapy, and creates challenges managing multiple providers involved in their care. Lack of illness knowledge and therapy can result in nonadherence, especially when symptoms aren’t present, stemming from unawareness of disease progression or the consequences of deviating from the medication regimen as prescribed. The Archives of Internal Medicine published that there’s a strong correlation between patients’ health literacy with knowledge of their illness. In addition, a lack of understanding of a therapy can influence patients’ trust and use of a medication.
Causes — The U.S. Dept. of Education reveals that adults with the lowest health literacy, numeracy and literacy skills self-reported the worst health of those assessed. Improving health literacy will have a positive estimated effect on patient health outcomes and can potentially reduce annual healthcare expenses by over $25 billion.
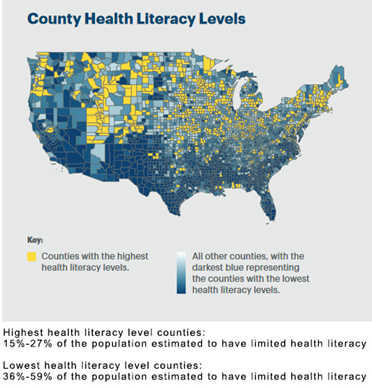
Variations in health literacy stem from differences in education, English proficiency, socioeconomic status and situational circumstances. The NAAL survey identified lower health literacy in adults 65 years of age and older, those with less education, and those who are medically underserved or uninsured.
Despite a prevalence of low health literacy in certain patient populations or areas, health literacy is also situational. Even those with proficient health literacy may not understand health information in certain circumstances, such as when they are sick, in pain or frightened. Or all of the above.
Ways to identify health literacy barriers to medication adherence
Identifying low health literacy enables pharmacists to employ communication strategies that empower patients to use medication the way it was intended. Low health literacy can affect anyone, so attempting to identify based on groups such as elderly or those on Medicaid or lacking insurance isn’t sufficient. Pharmacists should observe patient red flags for signs of low health literacy:
- Incompletely filled-out forms
- Missing medication refills for chronic conditions
- Medications are referred to by their shapes or colors
- Avoidance of reading printed material when in front of a pharmacist for reasons such as forgetting glasses or that the materials will be read with a spouse or child
- Mispronouncing words
- Presence of numerous folded papers in pockets or purse, or requesting more materials
- Lack of asking questions during the course of counseling
Ways to improve literacy and adherence
- Gain trust and create a supportive environment
Be aware that those with low health literacy may feel uncomfortable revealing their lack of understanding. Inadequate health literacy is associated with shame, causing patients to avoid asking questions or requesting that information be repeated or explained in a different way. Initially ask a patient what they know about a topic to assess their understanding. Ask open-ended questions in a respectful and caring tone that begin with “how” and “what;” avoid yes/no questions. Immediately engage the patient once low health literacy is identified, creating a welcoming environment where the patient feels comfortable. 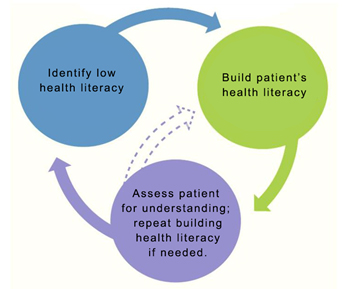 Apply the EDGE tactic: Explain, Demonstrate, Guide, Enable
Apply the EDGE tactic: Explain, Demonstrate, Guide, Enable
Explain the medication label and how to use the medication, device or therapy emphasizing 3 to 5 key points. Patients may recall or understand only 50% of a medical session. Refrain from using complex medical terms. Everyday Words for Public Health Communication from the CDC offers simpler word choices for medical terms.
Demonstrate how to take the medication, use a device, or follow a technique. Draw or show pictures and utilize audiovisual information as supplements to demonstration. MedlinePlus has audiovisual education on over 250 topics in 40 languages that can be suggested for patient reference.
Guide in a teach-back method, encouraging the patient to repeat or practice the technique during the counseling session to identify areas that need further instruction. Reinforce what they already know to instill confidence and motivation.
Confirm through the teach-back method, patient’s body language and communication that they understand and feel empowered to administer the therapy independently. Additionally, use an open-ended approach to address any final issues that could affect medication adherence such as “What questions do you have,” rather than “Do you have any questions?
3. Create a written materials repository…using the KISS method
Share written materials that help overcome information gaps not retained from consults. These materials can cover administration techniques, how to use devices, pictorial medication schedules, pharmacy forms, plain-language drug information sheets, and organizational instructions to build patient health/medication files for continuity of care between multiple providers.
Brochures and materials should be written in a simple, concise conversational style, available in different languages, and written at or below a sixth-grade level (in other words, keep it simple, silly!). The Flesch-Kincaid Readability Formula in Microsoft Word is a tool to calculate the readability of written materials. Ample white space should be left on the materials for patients to write notes, use fonts no smaller than 12 point, and include illustrations and pictures.
4. Collaborate with other healthcare providers
According to a study published in the Journal of American Pharmacists Association, physicians recognize that pharmacists have deeper and broader information on medication adherence information and thus are valuable collaborators. However, doctors and pharmacists alike have revealed time burdens, including schedule coordination, as a challenge.
Development of medication adherence forms, hard copy or integrated into pharmacy software, is a mechanism to quickly electronically send an alert to patients’ healthcare providers that inadequate health literacy or lack of illness and medication therapy (HowMed) knowledge was identified. The low-time-consuming alert can open a channel of communication and collaboration between the pharmacist and healthcare provider to improve patient health literacy and medication adherence. (When RxLive partners with a practice, our clinical pharmacists send an easy-to-read provider takeaway document for them to review, uploaded directly into the practice’s EHR after every patient consultation.)
Summary: Literacy a strong predictor of optimal health
Health literacy is a strong predictor of health, and pharmacists are critical to improving medication adherence in regards to this component of the understanding and knowledge bucket. Identification of inadequate health literacy is the initial opportunity to address medication adherence at the pharmacy level. We recommend creating a trusting, shame-free environment, employing EDGE tactics with teach-back, offering plain-language written materials, and collaborating with providers to help enable patients be adherent with their medication regimen by building their health literacy and illness and medication therapy knowledge.
Resources
Everyday Words for Public Health Communication. CDC
Relationship Between Patients’ Knowledge and Medication Adherence Among Patients with Hypertension. Patient Preference and Adherence
Low Medication Knowledge and Adherence to Oral Chronic Medications among Patients Attending Community Pharmacies: A Cross-sectional Study in a Low-income Country. BioMed Research International